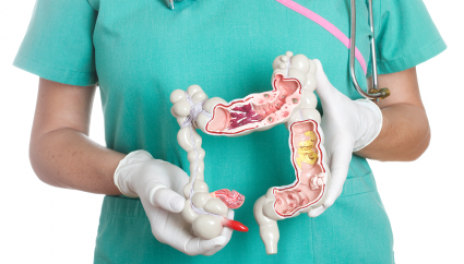
Ulcerative Colitis: Hemorrhagic ulcer disease, as well as Crohn’s disease, is a chronic intestinal inflammatory disease (IBD) of the colon and rectum. If Crohn’s disease can occur anywhere in the digestive tract and reach the tissues at depth, colitis Ulcer is a superficial involvement of the mucosa, which begins at the rectum to ascend into the colon.
There are four forms of ulcerative colitis, depending on the extent of the disease:
- Ulcerative proctitis, which confined to the rectum
- Proctosigmoiditis, which affects the rectum and the sigmoid colon
- Distal colitis, which affects the part of the colon on the left side of the body (from the rectum to the top of the descending colon)
- Pancolitis, which affects the entire colon
In Canada, it is estimated that almost two out of every 1,000 people (men, women, and children) have ulcerative colitis. In another country, France, the incidence of UC has decreased to 3.5 / 100,000 while it increases for Crohn’s disease. In Europe, it is 1.7 to 20.3 / 100 000 and is more frequent in northern Europe than in the south (Norway / Portugal gradient)
The disease is diagnosed, especially in people aged 30 to 40 years, but it can occur at any age. Men and women affected in almost the same proportions, but not at the same age. This could be related to the smoker or former smoker status. There is a female predominance for Crohn’s disease, a less pronounced masculine predominance.

Ulcerative Colitis: Causes
There is a genetic predisposition to ulcerative colitis. Hemorrhagic ulcerative colitis (HCV) is due to a dysregulation of the immune system that attacks the cells of its own organism. Scientists believe that the inflammation of the colorectal mucosa is due to an excessive immune reaction of the body against viruses or bacteria present in the intestine. According to the most probable hypothesis, this autoimmune reaction would be directed against the “harmless” bacteria normally present in the digestive tract (intestinal flora). EHR could also be related to environmental factors, not yet elucidated. Food stress and intolerance can trigger symptoms in some people, but these factors are not the cause of the disease.

Ulcerative Colitis: Complications
The hemorrhagic ulcer is associated with joint (axial or extremity) disorders, skin (erythema nodosum), inflammation of the eyes, or liver problems (sclerosing cholangitis). These disorders related to the autoimmune reaction involved in the disease. The most severe acute complication of ulcerative colitis called “toxic megacolon.” It occurs when inflammation of the colon is so severe that the colon dilates and is susceptible to perforation. This causes severe pain, fever, vomiting, and swelling of the abdomen. A doctor consulted urgently in the presence of these symptoms in order to prevent the colon from perforating and peritonitis from occurring. Fortunately, this complication rarely occurs (in less than 2% of cases).
People with ulcerative colitis should be aware of the risk of anemia. Indeed, when the disease is severe, abundant blood loss to the point of causing anemia, which compensated by iron supplements. Several complications related to the long-term use of certain drugs, such as corticosteroids or immunosuppressants, may occur. Thus, long-term use of corticosteroids increases the risk of osteoporosis, cataract, hypertension, type 2 diabetes, etc. Corticosteroids and immunosuppressants may also increase the risk of infection.

Ulcerative Colitis: Symptoms
The symptoms appear in seizures:
- Painful abdominal cramps, especially in the lower abdomen
- Blood in the stool (even hemorrhage in case of severe thrust)
- Chronic diarrhea
- Frequent stools, even during the night
- An urgent need to defecate, also if there is little or no stool to evacuate (rectal tenesmus)
- Weight loss due to reduced appetite and poor absorption of nutrients into the intestine
- Tiredness, often caused by anemia
- Fever, especially in the case of a pancolitis with significant symptoms;
- In children, severe ulcerative colitis can hinder development (delayed growth, delayed puberty, etc.).

Ulcerative Colitis: People at Risk
Some populations are more at risk than others because of their genetic inheritance. Whites are 2 to 5 times more affected by ulcerative colitis than Blacks or Asians. The Jewish community (of Ashkenazi origin) is 4 to 5 times more affected by this disease than other populations. Up to 20% of people with ulcerative colitis have a close family member with Crohn’s disease or only 6% with ulcerative colitis, suggesting a genetic predisposition. If two parents affected, the risk of the occurrence of IBD during life would be 36%.
Ulcerative Colitis: Risk factors
- Living in an urban environment or an industrialized country increases the risk of ulcerative colitis
- Non-steroidal anti-inflammatory drugs (NSAIDs, anti-inflammatory drugs other than corticosteroids) and oral contraceptives incriminated, but this remains confirmed. NSAIDs are not recommended for RCH
- Food factors are incriminated to the extent that this disease affects the countries of Europe and North America. (High consumption of sugar, red meat). The disease affects more and more the Maghreb, which reinforces the role of the food. (Modification of the diet in young people, soda, coca)
- Isotretinoin (Accutane), a drug used in the treatment of severe acne, may sometimes be involved in the onset of certain hemorrhagic rectocolitis.
- Although the causal relationship has not been proven, studies have reported cases of ulcerative colitis following the use of isotretinoin.

Ulcerative Colitis: Prevention
- Measures to prevent the disease
Since the precise causes of ulcerative colitis are still relatively vague, we can not prevent its occurrence. - Measures to prevent complications
People with inflammatory bowel disease recommended for five years or more to make an appointment with their gastroenterologist each year. Various tests are available to quickly detect abnormalities in the digestive tract, including colorectal cancer.
Prevention Measures
In the event of outbreaks of the disease:
- Dietary advice has no scientific validation. This disease is not food-borne, so it is unnecessary to impose food restrictions.
- Dietary advice is one of common sense.
- Do not take foods and drinks that aggravate your symptoms
- Avoid spicy foods, alcohol, some vegetables (cabbage, broccoli, beans), and drinks and foods that contain caffeine. These tend to cause bloating
- Pay particular attention to milk and certain dairy products, which trigger diarrhea, pain, and flatulence in some people with lactose intolerance. There is, however, no demonstrated link between lactose intolerance or milk protein allergy and ulcerative colitis.
- Limit intake of dietary fiber. Although dietary fiber is an essential component of a healthy diet, it often aggravates the symptoms of ulcerative colitis. Preferably consume cooked rather than raw fruits and vegetables;
- Eat several small meals during the day rather than 2 or 3 hearty;
- Consume a good amount of liquid, preferably water, avoiding carbonated drinks, alcoholic beverages and those containing caffeine;
- In the event of a serious crisis, doctors may also introduce a “no residue” regimen, excluding any source of plant fibers, animal residues, and greasy residues, to restore the colon for a few days during the outbreak.
Between periods of symptoms
- Consume foods rich in dietary fiber to regulate intestinal transit. Dietary fiber would also have the advantage of facilitating the growth of bacteria normally present in the intestines.
- It’s preferable to consume protein from lean meats, poultry, fish, and eggs. It is essential to adopt a healthy diet that contains good fats.
- Practice relaxation techniques and exercise to better manage your stress. If stress does not cause ulcerative colitis, it can aggravate its symptoms as it interferes with normal digestive functions. Exercise also helps to regulate intestinal transit. Relaxation methods can also help control pain in times of symptoms.


